Adrian Kwa describes the process of designing an app that allows doctors to access clinical guidelines quickly
Clinical guidelines are documents that provide guidance to clinicians when managing certain medical conditions. At Nottingham University Hospitals NHS Trust (NUH), there are just under 600 guideline documents stored on the NUH intranet system. To find the relevant guideline, users must first locate an available computer and log onto the system, then navigate through a myriad of links on the Trust website before arriving at the guideline page. The system is managed by non-clinical staff and documents are grouped by directorate ownership. The search function for this system yields many irrelevant results.
The system was not designed with the user in mind and is particularly impractical during medical emergencies, when it is both unsafe and time-consuming to leave the patient’s bedside to access the correct guidelines. The impracticality of the system has resulted in clinicians not following the Trust guidelines, a problem that could potentially affect patient safety and increase litigation risks. There have already been a number of recorded incidents of near-misses related to the accessibility of guidelines in the recent past.
Most staff carry a mobile phone during work, making them an ideal platform for the delivery of critical information at the bedside in a timely manner. There are already numerous websites and clinical apps on the market, and clinicians may choose to use these when treating patients. However, the quality of information cannot always be verified and may be different from Trust-approved guidelines. This lack of consistency could potentially impact on patient safety. We therefore decided to design and develop our own app to host Trust-approved clinical guidelines for all healthcare professionals within our Trust.
The main issue with the existing guidelines system was poor accessibility. We tackled this issue using a user-centred approach. We sent out an electronic questionnaire to all clinical staff within the Trust, gathering information about mobile phone ownership and use of other medical apps in their clinical practice. Around 520 clinical staff including doctors, nurses, midwives and physiotherapists responded to the survey. We learned that around 95% of staff own a smartphone, and over half the group have used it to access clinical information at least once a week. 89% of staff surveyed also said they would use a Trust clinical guidelines app if one was available.
Design specifications
The user interface for the app has to adapt to the fact that a smartphone does not have a separate keyboard or mouse. On-screen keyboards are difficult to type with, and the auto-correct feature on most devices would not recognise medical terminology. Therefore, we aimed to minimise the use of the keyboard, and the use of the search function.
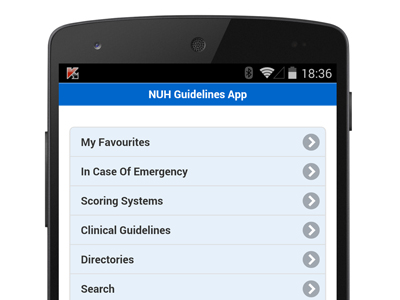
The menu system must be intuitive to navigate. From the outset, we set a target of making all documents accessible within three clicks of the home screen. The users must not be buried deep within layers of menu, so that even if they fail to navigate to their destination at first attempt, they can very easily find their way back.
We also created a section called ‘In Case of Emergency,’ where clinical guidelines for certain emergencies can be accessed quickly. Accessing this feature will take the user to an A to Z keypad. From here, users will only need to think of the name of the emergency, and click on the first letter of the name. This will take the user to final screen where the relevant guideline may be found.
The users are also able to create their own list of frequently-used guidelines within the app. In addition, there is a search function that will generate guidelines using relevant keywords. To mitigate the issue of mobile black-spots, the content is accessible offline, with features built-in to ensure it is always up to date.
User-centred design
We invited all clinical staff to attend focus groups meetings. In all, around 100 staff participated in separate sessions. During the meetings we ran card sorting exercises and critical incidents techniques. In discussion about the existing system, poorly designed interfaces and an over-powerful search function generating irrelevant results were identified as common problems.
For the card sorting exercise, we produced sets of cards with names of all current Trust guidelines. Participants were divided into groups and were asked to allocate these cards into the most relevant specialties. For guidelines that were deemed equally relevant in more than one group, extra cards were produced and the guidelines placed in all relevant groups. Participants were also asked to select guidelines that they thought should be located in the ‘In Case of Emergency’ section.
Field trial
Based on the findings during the focus groups, we developed a prototype app for field testing. The aim was to finalise the layout of the menu structure and assess usability. We developed a ‘Find the guidelines’ game, where participants have to find nine different guidelines and other information using the prototype app. None of the participants had used the app before and they were not provided with any instructions on how to use the app. No time limit was set for the test. They were asked not to use the search function, and to note down their first attempt. When the correct guidelines are found, instead of opening the document, the participants were presented with a six-digit code which they were asked to record on an answer sheet. There were multiple endpoints of each question, all with a unique code. If no guidelines were found, they were asked to record the location of where they had expected to find it. Using this model, a single investigator was able to run the trial with a large group of participants. At the end of the game, they were invited to give feedback on the design and their experience of using the prototype. We continued to modify the prototype during the testing period. Once the design was finalised we ran further tests and asked participants to score the app using the System Usability Scale (SUS).
Results
In all, a group of 102 participants, comprising doctors, nurses and midwives, participated in the initial field trial. We identified that all staff groups have different mental models when accessing guidelines. More experienced staff, including doctors and nurses, were more likely to use the ‘In Case of Emergency’ button for the clinical emergency questions, and were also more likely to use medical terminology when accessing this section of the app. It was difficult to identify the most appropriate locations for guidelines within the app.
Due to this difficulty, we redesigned the menu system so that most of the guidelines may be accessed from multiple locations within the main guidelines section, and where appropriate, via multiple points of entry in the ‘In Case of Emergency’ section as well. The app should be designed to fit all user groups, and the onus should be on us to identify the entry points suitable for each group.
Once the design was finalised, a new prototype was produced and we ran the test with a further 43 colleagues. All participants found the app intuitive to use, and were able find all guidelines easily. This finding is in keeping with the SUS Score of 83, placing it in the top 5th percentile.
Implementation
The app was made available on 31st July 2014. It features around 650 guidelines, with over 1300 points of entry. The guidelines are also searchable using one of 6500+ keywords.
In the first month, we recorded 763 downloads. The app has been accessed by around 82 unique users a day since launch. Based on the analytic data so far, less than 9% of hits used the search function as a point of entry, indicating the success of the menu design.
This is likely to be the first user-centred design system for managing clinical guidelines. We can see the potential this has in improving patient safety, and we aim to share our technology with other NHS Trusts across the country.
By Adrian Kwa
This article first appeared in The Ergonomist, No 533 November 2014